Contents
Overview
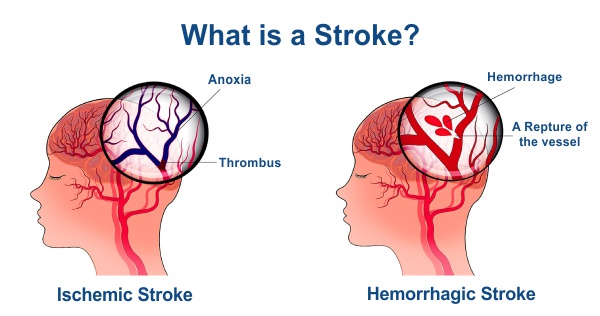
A life-threatening medical condition, stroke happens when the blood supply to part of the brain is cut off.
It may also occur when a blood vessel in the brain ruptures and bleeds, preventing blood and oxygen from reaching the brain’s tissues.
Without oxygen and nutrients, brain cells and tissue become damaged and die within minutes. This can cause lasting brain damage, long-term disability, or even death.
The sooner a person receives treatment for a stroke; the less damage is likely to happen.
What are the types of strokes?
There are three primary types of strokes:
- Transient ischemic attack (TIA) involves a blood clot that typically reverses on its own.
- Ischemic stroke involves a blockage caused by a clot or plaque in the artery. The symptoms and complications of ischemic stroke can last longer than those of a TIA or become permanent.
- Hemorrhagic stroke is caused by a burst or leaking blood vessel that seeps into the brain.
What happens during a stroke?
When brain cells die, brain function is lost. You may not be able to do things that are controlled by that part of the brain. For example, a stroke may affect your ability to move, speak, eat, think and remember, control your bowel and bladder, control your emotions or control other vital body functions.
The most common stroke symptoms are:
- Face – the face may drop on one side, you may not be able to smile, or your mouth or eye may drop.
- Arms – you may not be able to lift both arms and keep them there.
- Speech – your speech may be slurred, or you may not be able to talk at all despite appearing to be awake; you may also have problems understanding what others are saying to you.
Other signs and symptoms may include:
- complete paralysis of one side of the body
- sudden loss or blurring of vision
- dizziness
- confusion
- difficulty understanding what others are saying
- problems with balance and coordination
- difficulty swallowing (dysphagia)
- a sudden and very severe headache resulting in a blinding pain unlike anything experienced before
- loss of consciousness
Who is at risk for a stroke?
A stroke can happen to anyone at any time.
But some people have a greater chance of having a stroke. Some risk factors for stroke can be changed or managed, while others can’t.
Risk factors for stroke that can be changed, treated, or medically managed:
- High blood pressure
- Heart disease: the second most important risk factor for stroke. Heart disease and stroke have many of the same risk factors.
- Diabetes.
- Smoking: it almost doubles your risk for an ischemic stroke.
- Birth control pills (oral contraceptives)
- History of TIAs (transient ischemic attacks): TIAs are often called mini-strokes. They have the same symptoms as stroke, but the symptoms don’t last. If you have had one or more TIAs, you are almost ten times more likely to have a stroke than someone of the same age and sex who has not had a TIA.
- A high red blood cell count thickens the blood and makes clots more likely, raising the risk for stroke.
- High blood cholesterol and lipids: High cholesterol levels can contribute to the thickening or hardening of the arteries (atherosclerosis) caused by a buildup of plaque on the inside of the artery walls. This can decrease the amount of blood flow to the brain, causing a stroke.
- Lack of exercise
- Obesity
- Excessive alcohol use
- Drug abuse carries a high risk of stroke from blood clots (cerebral embolisms).
- Abnormal heart rhythm: Some types of heart disease can raise your risk for stroke. Having an irregular heartbeat (atrial fibrillation) is the most powerful and treatable heart risk factor of stroke.
- Cardiac structural abnormalities such as damaged heart valves (valvular heart disease) can cause long-term (chronic) heart damage. Over time, this can raise your risk for stroke.
- A family history of stroke or TIA.
- Age: Your risk of stroke increases as you get older.
How is a stroke diagnosed?
Your emergency team will try to determine what type of stroke you’re having at the hospital. Doctors also need to rule out other possible causes of your symptoms, such as a brain tumour or a drug reaction. You’ll have a CT scan or other imaging test soon after arrival.
Some of the tests include:
- You may have several blood tests, including tests to check how fast your blood clots, whether your blood sugar is too high or low, and whether you have an infection.
- A Computerized tomography (CT) scan uses a series of X-rays to create a detailed image of your brain. It can show bleeding in the brain, an ischemic stroke, a tumour or other conditions.
- Magnetic resonance imaging (MRI) uses powerful radio waves and magnets to create a detailed view of your brain. It can detect brain tissue damaged by an ischemic stroke and brain haemorrhage.
- Carotid ultrasound is done to get detailed images of the inside of the carotid arteries in your neck. This test shows the buildup of fatty deposits (plaques) and blood flow in your carotid arteries.
- An Echocardiogram creates detailed images of your heart and helps find the source of clots in your heart. The clots may have travelled from your heart to your brain and caused stroke.
What can I do to prevent a stroke?
Adopting a healthy lifestyle and knowing your stroke risk factors are the best steps you can take to prevent a stroke.
Many stroke prevention strategies are the same as strategies to prevent heart disease. In general, healthy lifestyle recommendations include:
- Controlling high blood pressure (hypertension)
- Lowering the amount of cholesterol and saturated fat in your diet
- Managing diabetes
- Quitting the use of tobacco
- Maintaining a healthy weight
- Eating a diet rich in fruits and vegetables
- Drinking alcohol in moderation
- Exercising regularly
- Treating obstructive sleep apnea (OSA)
- Saying no to drugs
Disclaimer:
This blog is for informational purposes only and should not be construed as advice or as a substitute for consulting a physician. It is not a substitute for medical advice or treatment from a healthcare professional.
Sources:


![Blood Test for Hair Loss [Male/Female] Blood Test for Hair Loss](https://oncquest-blog.s3.ap-south-1.amazonaws.com/blog/wp-content/uploads/2023/12/12044200/Blood-Test-for-Hair-Loss.webp)
