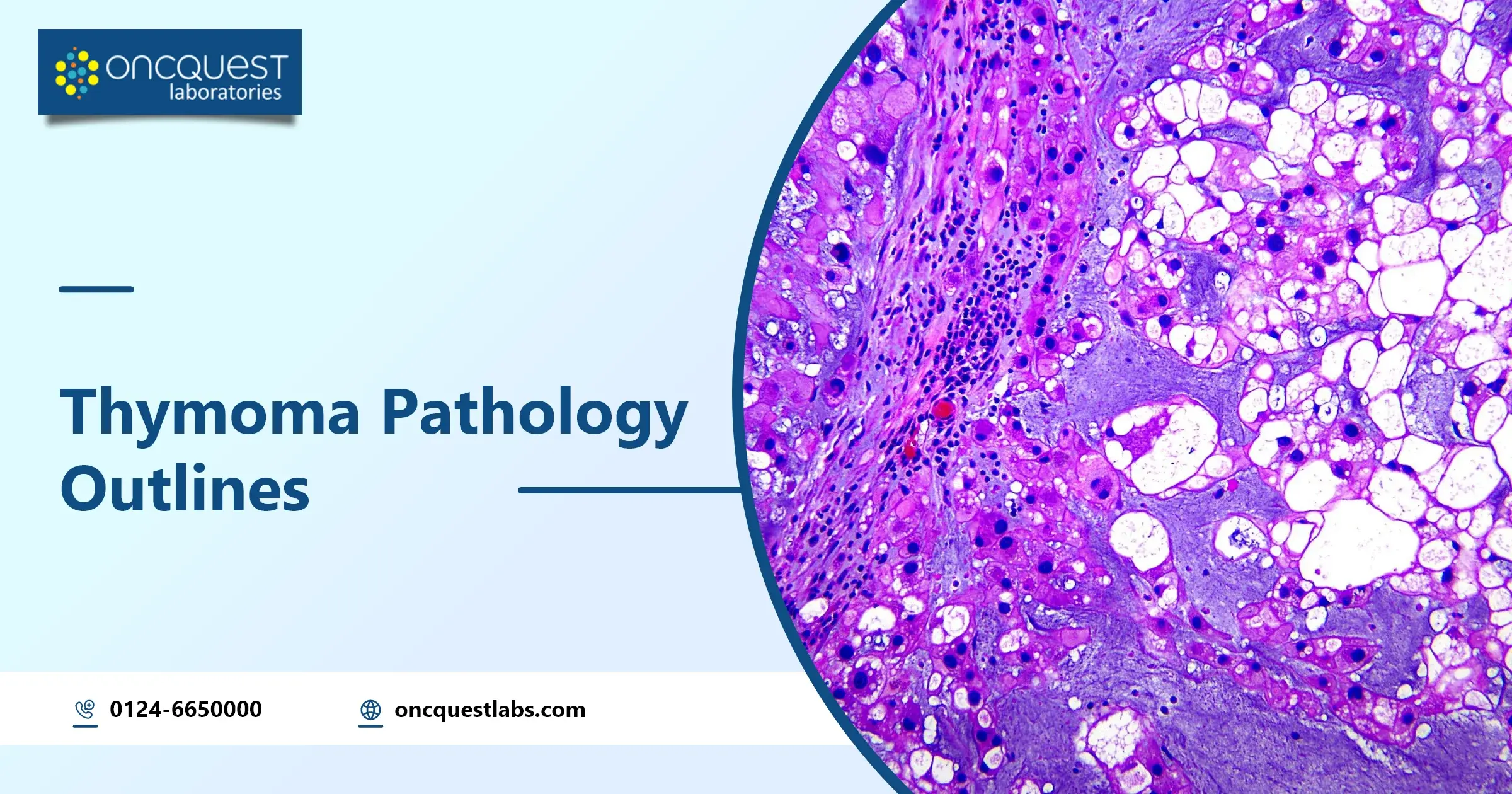
Thymomas are a sort of tumor found within the chest area, referred to as the mediastinum. They’re pretty rare, which makes professionals argue approximately how to call, classify, and level them effectively. For the past 20 years, there has been a debate about how vital it is to categorize thymomas based on their appearance under a microscope. A few experts think that knowing the degree of the tumor while it is identified is most vital, while others believe that knowing its appearance is vital for how patients will respond to treatment.
In this evaluation, we’ll communicate about the problems that pathologists face when reading thymoma tissues and figuring out their level. We will additionally, in short, discuss how these tumors behave and what treatments are currently used.
Contents
Overview of Thymoma
Thymic epithelial lesions, mainly thymomas, are a common cause of masses in the front part of the chest among adults. However, they’re pretty uncommon standards, making up about 0.2–1.5% of all malignant tumors. Among tumors in the front part of the chest (mediastinum), thymomas are the most common, accounting for approximately 20% of cases in adults. They arise at a charge of around 0.13–0.26 cases in keeping with one hundred,000 humans every year and are more common in human beings of their nineties and 1960s, with only 11% of instances identified earlier than age 35. Thymomas are barely more common in females than in men.
Sufferers with thymomas commonly present with an unmarried, nicely defined mass that can be effortlessly visible on CT scans. Maximum thymomas seem as rounded or oval lumps on MRI and CT scans. While calcification and bleeding areas are uncommon, any irregularities visible on CT scans can suggest that the tumor is invading nearby tissues or behaving aggressively.
Features of Thymoma
Thymomas can show up in specific ways. They might not show any signs and are observed incidentally on chest x-rays in approximately one-third of instances. In other instances, they can cause symptoms like chest ache, a lump inside the neck, or a circumstance referred to as superior vena cava syndrome, which occurs when a massive vein in the chest is compressed.
It’s vital to notice that thymomas are linked to different clinical conditions known as paraneoplastic illnesses. These consist of autoimmune disorders, collagen vascular issues, blood problems, and others. The most powerful connection is with myasthenia gravis (mg), which’s found in approximately 10–15% of thymoma instances. Additionally, some sufferers with M.D. and thymoma may additionally produce other autoimmune illnesses.
A surgical procedure is the preferred remedy for thymomas, especially if the tumor hasn’t spread an awful lot. But the quantity of the tumor’s spread and whether or not it could be absolutely removed are vital factors in determining the treatment method. For much less invasive tumors, surgery on my own can be enough; however, more aggressive cases might need extra remedies like chemotherapy or radiation. Even after a surgical operation, thymomas can come again, so long-term follow-up is crucial. Recurrences can arise in approximately 10–29% of instances, frequently spreading to the lungs, liver, or bones.
Classification of Thymoma
| Topic | Classification |
| Thymoma Classification Challenges | Thymomas are hard to classify due to their diverse nature and the difficulty in predicting outcomes based on specific cell types. |
| Early Classification Attempts | Bernatz et al. in 1961 categorized thymomas based on lymphocyte and epithelial cell ratios. Marino and Muller-Hermelink’s 1985 classification focused on mimicking healthy thymic structures. |
| World Health Organization (WHO) Classification | The WHO’s 1999 classification divided thymomas into type A (spindle/oval cells), type B (round/epithelioid cells), and type AB (mix). Type B thymomas are further classified into B1, B2, and B3 based on cell characteristics and atypical. |
| Suster-Moran Proposal | Suster and Moran’s 1999 proposal graded thymic neoplasms based on differentiation levels: well-differentiated thymomas, atypical thymomas, and thymic carcinomas. |
| Pathological Features | Thymomas can vary in size and macroscopic characteristics like solid or cystic. Microscopically, they exhibit different growth patterns that can be diagnostic challenges. |
| Unusual Histologic Subtypes | Various unusual histologic subtypes exist, including micronodular thymoma with B-cell lymphoid hyperplasia, plasma cell-rich thymoma, and metaplastic thymoma. These variants pose diagnostic challenges and require appropriate treatment. |
More About Characteristic of Thymoma
| Topic | Characteristic |
| Immunohistochemical Characteristics | – No established unique immunohistochemical marker for thymic epithelial cell malignancies. – Epithelial component usually positive for broad-spectrum cytokeratin, cytokeratin 5/6. – T-cell component highlighted by CD45 and TDT. – Occasional expression of markers like PAX8, calretinin, TTF-1, CD5, CD117, synaptophysin, CD56, PD-L1. – Generally negative for monoclonal PAX8 and EMA. |
| Role of PD-L1 in Thymomas | – High PD-L1 expression associated with advanced Masaoka staging and high-grade histology. – Studies show conflicting results regarding its prognostic value. – PD-L1 expression observed in up to 82% of thymic epithelial neoplasms. – Supports potential for PD-1/PD-L1 targeted treatment but prognostic predictive value remains uncertain. |
| Molecular Profile of Thymomas | – Low mutational burdens with various copy number abnormalities. – Common molecular alterations: loss of heterozygosity on chromosome 6, GTF2I mutations (especially p.L424H in type A/AB thymomas), NRAS and TP53 mutations (predominantly in type B2/B3 thymomas and thymic carcinomas), HRAS mutations (mainly in type A/AB thymomas).- No targetable mutations like EGFR or KIT genes identified. |
| Thymoma Staging Systems | – Historical staging by Masaoka (1981) based on severity (Stage I to IV). – Koga-modified Masaoka staging system commonly adopted, emphasizing invasive criteria. – Recent user-friendly staging systems consider anatomical penetration, precise tumor involvement, and mode of spread. – Moran et al. ‘s staging system designed for detailed anatomical region information to guide treatment decisions. – AJCC TNM proposal incorporates tumor capsule integrity and invasion into adjacent structures for staging. |
Treatment for Thymoma
•Surgical elimination is the only treatment for thymomas, imparting high survival charges, specifically in stage i and ii thymomas.
•The surgical procedure commonly involves an average sternotomy and a complete thymectomy to dispose of the tumor.
•For more invasive tumors (masaoka stage iii), surgical treatment may involve resection of surrounding tissues like the pericardium, lung, or hemidiaphragm.
•Numerous surgical approaches may be used, including minimally invasive strategies like video-assisted thoracoscopic surgical procedures or robot surgical treatment.
•Chemotherapy is powerful for thymomas, with reaction quotes starting from 30% to 60% for domestically advanced cases.
•Cisplatin-primarily-based regimens are normally used.
•Radiation therapy can also be used, especially for invasive thymomas, to improve neighborhood tumor control and decrease recurrence fees.
•For thymoma recurrences or advanced cases, multimodal treatments combining surgery, radiation, and chemotherapy are advocated for better outcomes.
•Techniques like hyperthermic intrathoracic chemotherapy (hithoc) after surgical excision have proven effective in handling local sickness and enhancing survival rates.
Where to Diagnose for Thymoma?
Oncquest Labs is the best and renowned pathology lab where you get tested for thymoma. CT scan and MRI both are available in Oncquest Labs. Oncquest Labs provides advanced pathology services for accurate histological examination and immunohistochemical analysis to confirm the diagnosis of thymoma.
Frequently asked Questions
Q1: Is thymoma benign or malignant?
A1: A thymoma is a cancerous tumor that typically originates in the prevascular mediastinum but can also occur in various locations such as the neck, pulmonary hilum, thyroid, lung, pleura, or pericardium.
Q2: What is the histology of thymoma?
A2: Epithelial cells with varying shapes like polygonal, stellate, and spindle are observed, along with predominantly T lymphocytes. The epithelial cells show positivity for CK7, CK5/6, P63, P40, CD205, Foxn1, and PAX8.
Q3: WHO classification of thymoma?
A3: Thymomas are categorized based on histologic features into type A thymoma (including an atypical variant), AB thymoma, type B thymoma (further divided into B1, B2, and B3 thymomas), micronodular thymoma with lymphoid stroma, and metaplastic thymoma. Rarely, immunohistochemistry such as immature T cell content is also considered for classification.
Q4: What are the cytological features of thymoma?
A4: Thymoma cytology is characterized by two main cell types: lymphocytes and epithelial cells. However, this similarity can lead to a broad range of potential diagnoses, including benign thymic lesions and metastatic carcinoma in a mediastinal lymph node.
Q5: What is the staging of thymoma?
A5: Stage I – The tumor remains within the thymus without spreading to the outer layer.
Stage IIA – The tumor is starting to invade the outer layer of the thymus or nearby tissues.
Stage IIB – The tumor has grown into the outer layer of the thymus or nearby tissues.