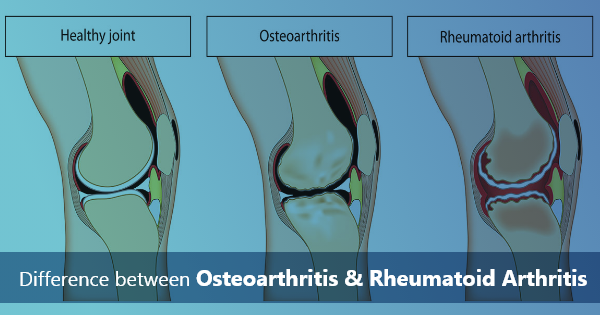
Arthritis is a term that encompasses a wide range of joint diseases, with two of the most common types being Osteoarthritis (OA) and Rheumatoid Arthritis (RA). While both conditions affect the joints and can cause pain and discomfort, they differ significantly in their causes, symptoms, and treatments. In this blog, we will explore the key differences between Osteoarthritis and Rheumatoid Arthritis to help you better understand these prevalent musculoskeletal disorders.
Contents
1. Causes:
Osteoarthritis:
– Osteoarthritis is primarily a degenerative joint disease.
– It occurs when the protective cartilage that cushions the ends of bones wears down over time.
– Aging, joint injuries, and obesity are common risk factors.
Rheumatoid Arthritis:
– Rheumatoid Arthritis is an autoimmune disorder.
– It happens when the immune system mistakenly attacks the synovium, the lining of the membranes that surround the joints.
– Genetic and environmental factors can contribute to its development.
2. Symptoms:
Osteoarthritis:
– OA typically causes joint pain, stiffness, and swelling, especially after physical activity.
– Pain tends to worsen over time and is often more severe at the end of the day.
– Affected joints may become less flexible, and there can be the development of bone spurs.
Rheumatoid Arthritis:
– RA often results in joint pain and stiffness that is more symmetrical, affecting both sides of the body equally.
– Morning stiffness lasting for more than an hour is a hallmark symptom.
– RA can also lead to systemic symptoms such as fatigue, fever, and weight loss.
3. Joint Involvement:
Osteoarthritis:
– OA typically affects weight-bearing joints such as the knees, hips, and spine.
– It can also impact the fingers, especially the ones closest to the nail.
Rheumatoid Arthritis:
– RA can affect any joint, including smaller joints like those in the hands, wrists, and feet.
– It can also affect non-joint structures, such as the heart, lungs, and blood vessels.
4. Diagnosis:
Osteoarthritis:
– Diagnosis is often based on medical history, physical examination, and imaging studies like X-rays.
– Blood tests are generally not used to diagnose OA.
Rheumatoid Arthritis:
– RA is diagnosed through a combination of physical examination, blood tests (specifically for rheumatoid factor and anti-CCP antibodies), and imaging studies.
– Early diagnosis is crucial for timely treatment to prevent joint damage.
5. Treatment:
Osteoarthritis:
– OA management focuses on pain relief and improving joint function.
– Treatment includes lifestyle modifications, physical therapy, pain medications, and, in severe cases, joint replacement surgery.
Rheumatoid Arthritis:
– RA treatment aims to suppress the immune system’s abnormal response.
– Medications like disease-modifying anti-rheumatic drugs (DMARDs) and biologics are commonly prescribed.
– Early and aggressive treatment can slow disease progression and preserve joint function.
Conclusion:
In summary, Osteoarthritis and Rheumatoid Arthritis are distinct conditions with different causes, symptoms, and treatment approaches. While Osteoarthritis is primarily a result of wear and tear on the joints, Rheumatoid Arthritis is an autoimmune disease. Understanding these differences is essential for accurate diagnosis and effective management of these chronic conditions. If you suspect you may have arthritis symptoms, consult a healthcare professional for proper evaluation and guidance tailored to your specific needs.
Frequently asked Questions
Q1:Which is more serious, osteoarthritis or rheumatoid arthritis?
A1:Osteoarthritis (OA) typically targets a smaller number of joints, and its symptoms primarily manifest within those joints. In contrast, the course of Rheumatoid Arthritis (RA) is often less predictable, and it can give rise to more widespread symptoms affecting various parts of the body. Thanks to ongoing research and advancements in therapies, the prognosis for individuals with RA has significantly improved, offering hope for better management of this condition.
Q2:What is the difference between osteoarthritis and rheumatoid arthritis on an x-ray?
A2:Furthermore, your doctor may request a series of diagnostic imaging tests, such as X-rays, MRI scans, and ultrasound scans, to validate the diagnosis and assess the precise location and severity of your arthritis. In X-rays, the appearance of joints affected by Rheumatoid Arthritis (RA) differs from those affected by Osteoarthritis (OA). In cases of OA, the images typically reveal reduced space between the bones and more noticeable erosion in RA-affected joints.
Q3:Can osteoarthritis be mistaken for RA?
A3:While Osteoarthritis (OA) and Rheumatoid Arthritis (RA) may exhibit overlapping symptoms, RA tends to involve multiple joints symmetrically, affecting both sides of the body. Conversely, OA typically targets only a limited number of joints, usually on one side of the body. Additionally, RA can produce flu-like symptoms like fever and a general sense of unwellness (malaise), distinguishing it from OA.